Atrial Fibrillation vs Ventricular Fibrillation – High‑Yield Review
Target audience: MBBS doctors preparing for NEET PG / INI‑CET / CMS.
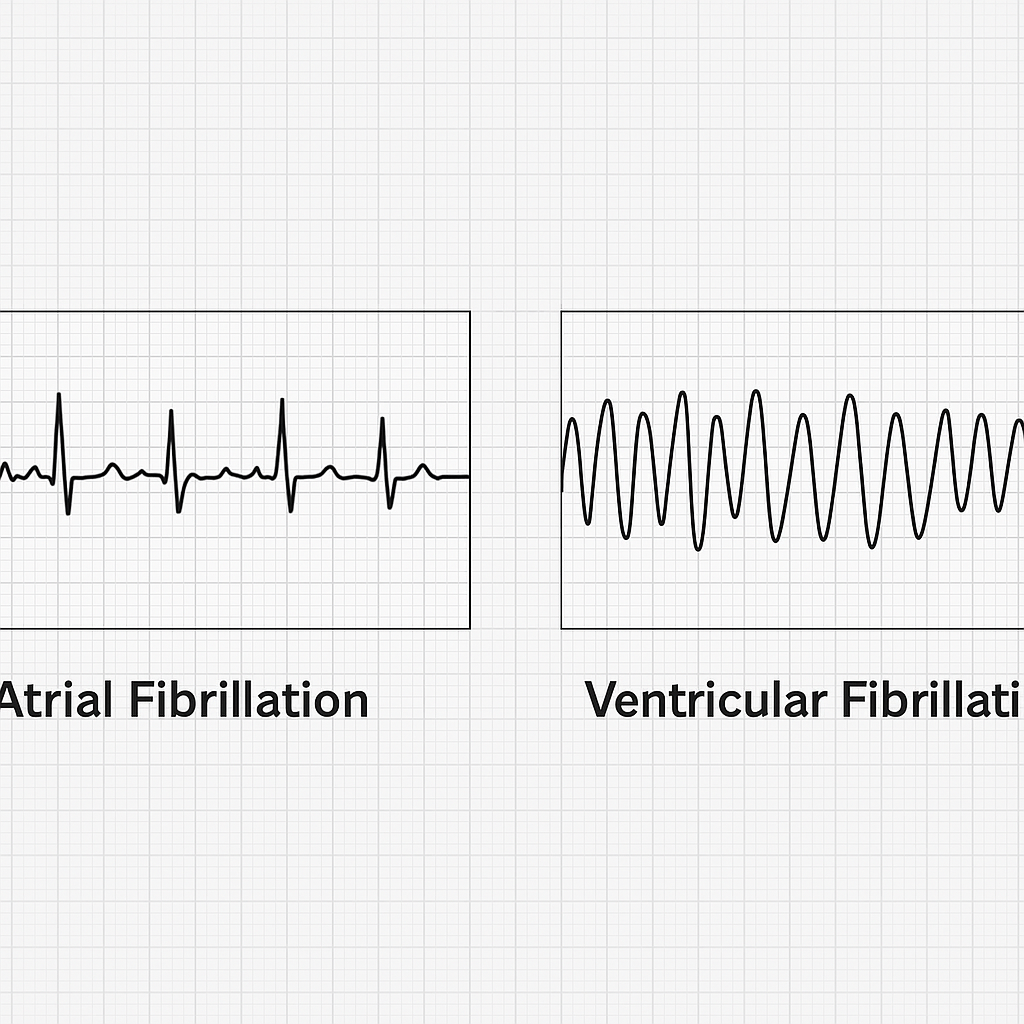
Atrial fibrillation (AF) and ventricular fibrillation (VF) are commonly tested arrhythmias with entirely different clinical urgency. AF is usually compatible with life but carries long‑term thromboembolic risk, whereas VF is immediately fatal unless treated within minutes. This short note focuses only on exam‑relevant and bedside‑relevant facts. Jump to Test Yourself (MCQs)
Atrial Fibrillation (AF)
- Definition: Chaotic atrial electrical activity causing loss of coordinated atrial contraction and an irregularly irregular ventricular rhythm.
- Common causes: Hypertension, coronary artery disease, rheumatic mitral stenosis (classic), hyperthyroidism, alcohol (“holiday heart”), post‑cardiac surgery.
- ECG hallmarks: Absence of P waves, presence of fibrillatory (f) waves, irregular RR intervals, usually narrow QRS.
- Hemodynamic effect: Loss of atrial kick → reduced cardiac output, more significant in elderly and diastolic dysfunction.
- Major complication: Thromboembolism, especially ischemic stroke due to clot formation in the left atrial appendage.
- Management principles:
- Rate control: β‑blockers, diltiazem, verapamil; digoxin preferred in heart failure.
- Rhythm control: amiodarone or electrical cardioversion in selected patients.
- Anticoagulation guided by CHA₂DS₂‑VASc score.
- Definitive option: catheter ablation (pulmonary vein isolation).
Ventricular Fibrillation (VF)
- Definition: Rapid, disorganized ventricular electrical activity resulting in no effective cardiac output.
- Most common cause: Acute myocardial infarction.
- Other causes: Hypoxia, acidosis, hypokalemia, hypomagnesemia, drug toxicity, cardiomyopathy.
- ECG features: Completely chaotic waveform with no identifiable P waves, QRS complexes or T waves.
- Clinical presentation: Sudden cardiac arrest – patient is pulseless and unconscious.
- Management:
- Immediate defibrillation – single most important life‑saving step.
- High‑quality CPR.
- Epinephrine and amiodarone.
- Post‑ROSC: identify reversible causes and consider ICD for secondary prevention.
AF vs VF – Key Exam Differences
| Feature | Atrial Fibrillation | Ventricular Fibrillation |
|---|---|---|
| Chamber involved | Atria | Ventricles |
| Pulse | Present, irregular | Absent |
| Immediate risk | Stroke | Sudden death |
| ECG | No P waves, irregularly irregular | Chaotic baseline |
| First‑line action | Rate control + anticoagulation | Defibrillation |
High‑Yield Clinical Pearls
- AF is never an indication for emergency defibrillation unless associated with instability.
- VF should never be treated with drugs before attempting defibrillation.
- Always think of AF when the pulse is irregularly irregular.
Take‑home message: AF is a chronic arrhythmia with thromboembolic implications; VF is an electrical catastrophe requiring instant shock. Confusing the two in exams or emergencies can be fatal.
© atsixty.com – concise medical notes for postgraduate entrance preparation.
Test Yourself: Atrial vs Ventricular Fibrillation
Quick revision MCQs for NEET PG / INI-CET
⏰ Quiz Not Available Right Now
Available daily from 10:00 AM to 5:00 PM.
Please come back during that window.